How To Reduce COVID-19 Spread At Long-Term Care Facilities
It’s well documented that people over 65 and those with underlying medical conditions are at most risk for severe illness from COVID-19. But throughout the early stages of the pandemic, overcapacity at many hospitals forced states to mandate moving coronavirus patients to long-term care facilities with open availability.
Visitor sign-in badges, "screened" labels and color code labels make it easy to distinguish the staff, volunteers and guests that have been checked in properly.
Unfortunately, moving COVID-19 patients into locations with the most vulnerable population, combined with a lack of personal protective equipment (PPE) and consistent infection prevention processes, led to avoidable infections and deaths. Fortunately, these experiences provide a clearer understanding of the challenges nursing homes faced and identified processes that will help control the virus in the future.
Screening & Visitor Management
As the coronavirus outbreak grew, many long-term care facilities enacted visitor restrictions and started daily screening of essential staff. And until there is a vaccine or the virus subsides, these controls will remain essential. In addition, facilities observed the importance of ongoing communications that informed stakeholders that processes and protocols were being followed.

Whether the test occurs in a hospital, commercial, private or academic lab, or a state testing facility, a COVID-19 specimen label is one of the required components.
Testing
Increasing patient and visitor flexibility in nursing homes will likely require regular testing. For example, CMS recommends nursing homes do not advance through any of the stages of reopening or relax any restrictions until all residents and staff have received a baseline test to establish that there are no known cases of COVID-19 in the facility.
Further, if a resident or staff member has symptoms consistent with COVID-19 or one tests positive for it, then additional testing is necessary. And, retesting should occur until all residents test negative.
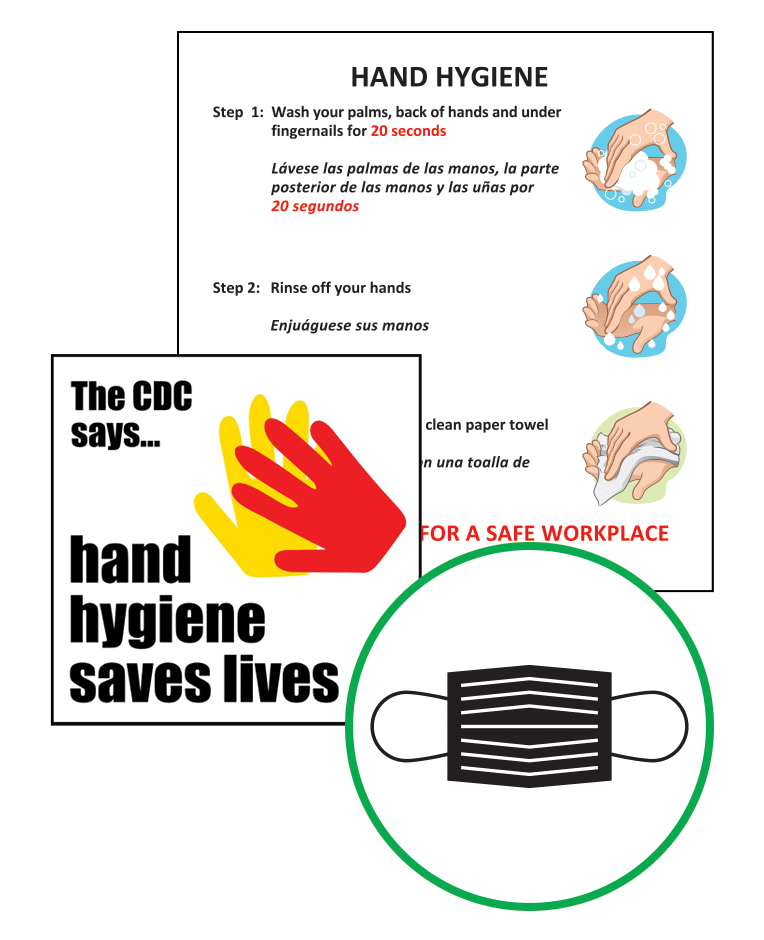
Placing signs in high traffic locations within your facility reinforces those messages and helps combat the virus's spread.
In addition, to execute the testing, a long-term care facility must determine whether they are capable of collecting specimens or require support. The testing methods might include a local hospital lab using high-throughput testing, working with state labs, or point-of-care tests as they become available.
Hand Hygiene
Nursing staff can touch up to 15 different surfaces during a single patient interaction. This means a nurse caring for five patients touches up to 900 surfaces per 12-hour shift.
Although hand and respiratory hygiene communications are now fairly common, reinforcing infection prevention and control measures from hand and respiratory hygiene to selection and correct use of PPE is still important. This is especially effective with new staff members and patients. Plus, demonstrating proper PPE use and monitoring adherence will improve compliance.
Communal Dining Restrictions
When facilities reopen to more normal activities, it’s crucial to maintain strict guidelines. For example, social distancing measures such as remaining at least six feet apart, face coverings, if tolerated, and hand hygiene continue to be essential practices.
In addition, for patients that require isolation or if communal dining restrictions are necessary, it may be necessary to divert to in-room meal delivery.
United Ad Label
UAL’s label and healthcare knowledge help to elevate communications and aid long-term care facilities and nursing homes as they return to some level of standard operating procedures. Contact us to learn more.
¹ Yourish K, Lai KKR, Ivory D, Smith M. One-third of all U.S. coronavirus deaths are nursing home residents or workers. New York Times. May 9, 2020.
