Blog Post Updated 11/30/2024
Orginal Publish Date 6/26/2018
A Johns Hopkins study suggests medical errors are the third leading cause of deaths in the U.S.
The Journal of General Internal Medicine believes the number of preventable deaths are just over 22,000.
Regardless of which statistic you believe is more accurate, consistently executing effective patient safety remains an ongoing challenge. And although it’s embedded into the processes and procedures of all health systems, faculty at the Harvard School of Public Health characterized patient safety improvements in hospitals as “excruciatingly slow.”
But, for patient safety improvements to occur, it's essential to identify the hot spots and define potential solutions. That's the purpose of the national patient safety goals.
What Are National Patient Safety Goals?
The Joint Commission publishes national patient safety goals to bring focus to patient safety challenges throughout the spectrum of care. These are the 2025 patient safety goals for each care area.
- Ambulatory National Patient Safety Goals
- Assisted Living Community National Patient Safety Goals
- Behavioral Healthcare and Human Services National Patient Safety Goals
- Critical Access Hospitals National Patient Safety Goals
- Home Care National Patient Safety Goals
- Laboratory National Patient Safety Goals
- Hospital National Patient Safety Goals
- Nursing Care Center National Patient Safety Goals
- Office Based Surgery National Patient Safety Goals
- Rural Health Clinic National Patient Safety Goals
- Telehealth National Patient Safety Goals
How Often Are National Patient Safety Goals Updated?
Each year, The Joint Commission updates the NPSG goals. And, if you compare them with past years, you’ll see many similarities, which speak to the challenges these patient safety issues create for healthcare providers.
What Are National Patient Safety Goals Based On?
The NPSG goals are regularly revised based on their impact, cost and effectiveness. In addition, regardless of the care area, you’ll see these consistent themes as you read through each publication. These include:
- Patient identification accuracy
- Caregiver communication
- Medication safety
- Clinical alarm systems
- Infection prevention
- Surgery verification
- Identify patient safety risks
- Improve healthcare equity
But, as important as these goals are as a starting point, improving patient safety requires a system wide commitment and a continuous improvement mindset. Yet the steps necessary to make these improvements are far simpler than the complexities typical of the patient care process - although they are still difficult to achieve. In addition to internal systems, medical devices and the diligence of the clinical staff you deploy today, using tactics like those described below, ranging from double checking patient and medication information to using healthcare labels to guide communications, can help to improve patient safety throughout your operation.
2025 Joint Commission National Patient Safety Goals
1. Improve the Accuracy of Patient Identification
Patient identification mistakes can lead to errors in a variety of areas including:
- Medication administration
- Failure to treat a serious illness or disease
- Medical treatment for erroneous diagnostic lab results
- Performing procedures on the wrong patient
... and more. That makes using two forms of identification critical to ensuring patients get the correct medication and treatments. In addition, patients often identify themselves by their middle name or a nickname instead of the name on their patient record so those two identifiers should include the patient’s full name, date of birth and/or medical identification (ID) number for every patient encounter.
Admission Labels And Wristbands Help You Achieve Effective Patient Identification
Admission labels and wristbands are the first step in patient identification and the foundation of patient safety in hospitals. They provide positive patient identification and communicate important information to the medical staff including allergies, fall risk and other medical alerts.
2. Improve Effectiveness of Communication Among Caregivers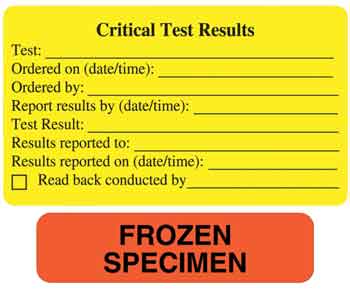
Diagnostic tests are essential to identifying the cause of patients' symptoms and determining the appropriate course of treatment. Delivering important test results to the right person in a timely manner is critical to the process.
Communication Labels Help Direct Effective Processes
Communication labels capture and convey important results for quick action. They simply impart information and ensure a greater understanding of processes.
3. Improve the Safety of Using Medications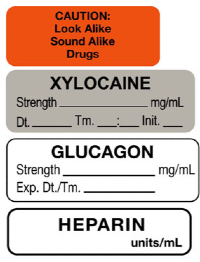
The Agency For Healthcare Research And Quality reports that nearly 5% of hospitalized patients experience an Adverse Drug Event (ADE) making them one of the most common types of inpatient errors. Further, ambulatory patients may experience ADEs at even higher rates. Medicines that are not conventionally labeled are common culprits. This includes medicines in syringes, cups and basins. If medications or other solutions remain unlabeled, they are unidentifiable which can result in errors, sometimes tragic.
Anesthesia Drug Labels Aid Effective Medication Dispensing
Unlabeled containers that look alike, drugs names that sound alike, and illegible handwriting create medication dispensing challenges. Anesthesia drug labels help prevent confusion and misidentification. For example, printed medication names eliminate errors resulting from illegible handwriting. And for prepared medications, labels allow the medical staff to record key data points, such as drug name, strength and more, to aid in proper dispensing. In addition, anesthesia drug labels highlight medications that have been added to IVs, helping to prevent dispensing errors and overdosing.
Labeling medications is not a one size fits all process. Read more on How To Label Medications Properly
4. Reduce Patient Harm Associated With Clinical Alarm Systems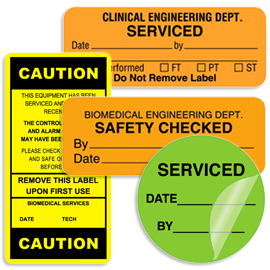
The numerous alarm signals throughout patient care areas that result in noise and displayed information can create an overall desensitization to those alerts. The unfortunate outcome is it may cause the staff to miss, ignore or even disable alarm signals! In addition, other challenges include too many devices with alarms, default settings that are not at an actionable level, and alarm limits that are too narrow. But that's not all...
Alarms Can’t Be Heard If They Don’t Work
Although there are no universal solutions, but developing a systematic, coordinated approach to clinical alarm system management is a good starting point. And once the approach is defined, ensuring the alarms work is another essential piece of the puzzle. Biomedical clinical engineering labels help health systems track and communicate important safety, maintenance, calibration and inspection information to ensure that alarms sound when needed.
Preventive maintenance is the best way to prevent equipment failures. Read More on How To Reduce Equipment Failures and Repair Costs
5. Reduce the Risk of Healthcare-Associated Infections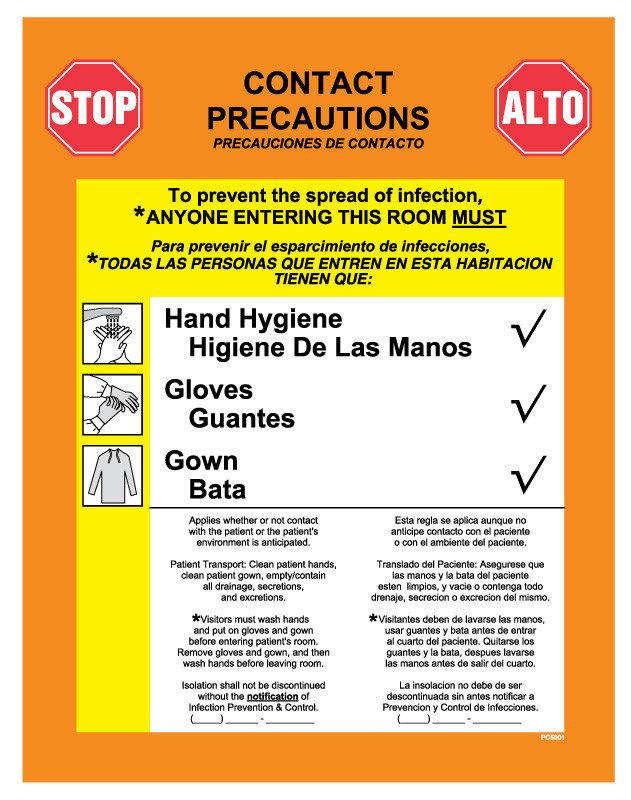

A JAMA Internal Medicine research study found that although hand hygiene compliance reached more than 90% during the peak of the pandemic, in just over a year, many healthcare workers regressed to previous habits. Overall compliance dropped back to 2019 levels “averaging 50 percent across hospitals nationwide.
It’s clear that regardless of all the data that highlights its importance, effective infection prevention programs remain an elusive goal. In fact, it takes a system wide commitment and an ongoing focus on proccesses and protocols to maintain high levels of compliance. Plus, as difficult as it is to maintain compliance, the best solutions aren't complex.
Hand Hygiene Prevents The Spread Of Infections
According to the CDC, hand hygiene is the simplest approach to preventing the spread of infections. Electronic monitors and observation tools can lead to higher levels of compliance. Plus, placing infection control signs and labels in high traffic areas inform and guide staff, patients and visitors to take appropriate precautions.
Use These 6 Steps For Effective Infection Prevention Programs
6. Conduct a Preprocedure Verification Process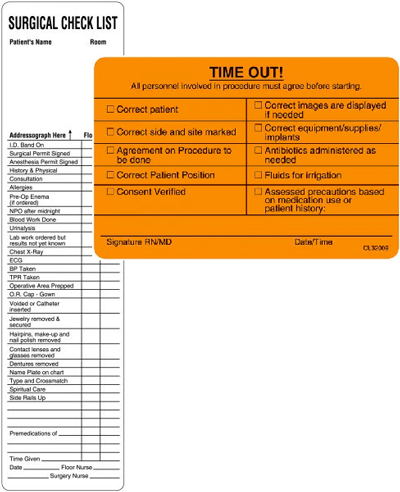
General anesthesia or deep sedation is necessary for most major operations. And although these lifesaving or life-changing procedures aren't possible without it, evidence indicates that it's also what places the patient at the most risk. That's why it's essential to use multiple, complementary strategies to ensure you conduct the correct procedure on the correct person, at the correct site.
Preprocedure Verification Process
The routine tasks of surgeons have become incredibly complicated. Missing a step, forgetting to ask a key question or, in the stress and pressure of the moment, failing to plan properly for every eventuality is almost inevitable. If you don't use a preprocedure verification process. It ensures that all relevant documents and related information or equipment are correctly identified, labeled, and matched to the patient’s identifiers prior to the start of the procedure. This includes reviewing the procedure and site with the patient and care team to verify the accuracy. The consistent implementation of a standardized protocol is most effective in achieving safety. Checklists are an important part of standardized protocols, and when implemented consistently, are effective in achieving surgical safety.
United Ad Label
United Ad Label develops products that aid and enhance patient safety processes in health systems, hospitals, clinics, physician offices, nursing homes and more. If your protocol requires a different message, color or process that UAL stock products do not address, check out our custom solutions. We can create a label that meets your exact needs and bring awareness to the Joint Commission patient safety goals. Click here to learn more.
Editors Note: This post was updated in November, 2024 to reflect the latest NPSG information from The Joint Commission.


